Bioprinting 6 Groundbreaking Developments
The world of advanced medical technology is undergoing a revolution that melds living tissue with cutting‐edge manufacturing methods. In this article, you will discover how a blend of history, innovative research, and future predictions is paving the way for enormous breakthroughs.
This blog post is written for a broad audience—whether you’re a student, researcher, or curious reader—using clear language and engaging examples to explore the transformative potential of advanced living tissues creation. You’ll learn about the evolution from early 3D technologies to modern systems that mimic natural tissue complexity.
Read on to find out how this technology integrates multidisciplinary insights from biology, engineering, and materials science, and join the conversation on its promising future in healthcare.
📑 Table of Contents
- Introduction to Bioprinting
- Evolution and History of Bioprinting
- How 3D tissue printing Enhances Bioprinting
- Bioprinting: Organ Fabrication Systems and Their Applications
- Real-World Case Studies of Bioprinting
- Medical Manufacturing in Modern Bioprinting Solutions
- Future Trends in Bioprinting: Cell Scaffold Printing and Beyond
- Bioprinting Insights: A Glimpse into Future Possibilities
- FAQ
- Conclusion
Introduction to Bioprinting
Foundations and Technology Overview
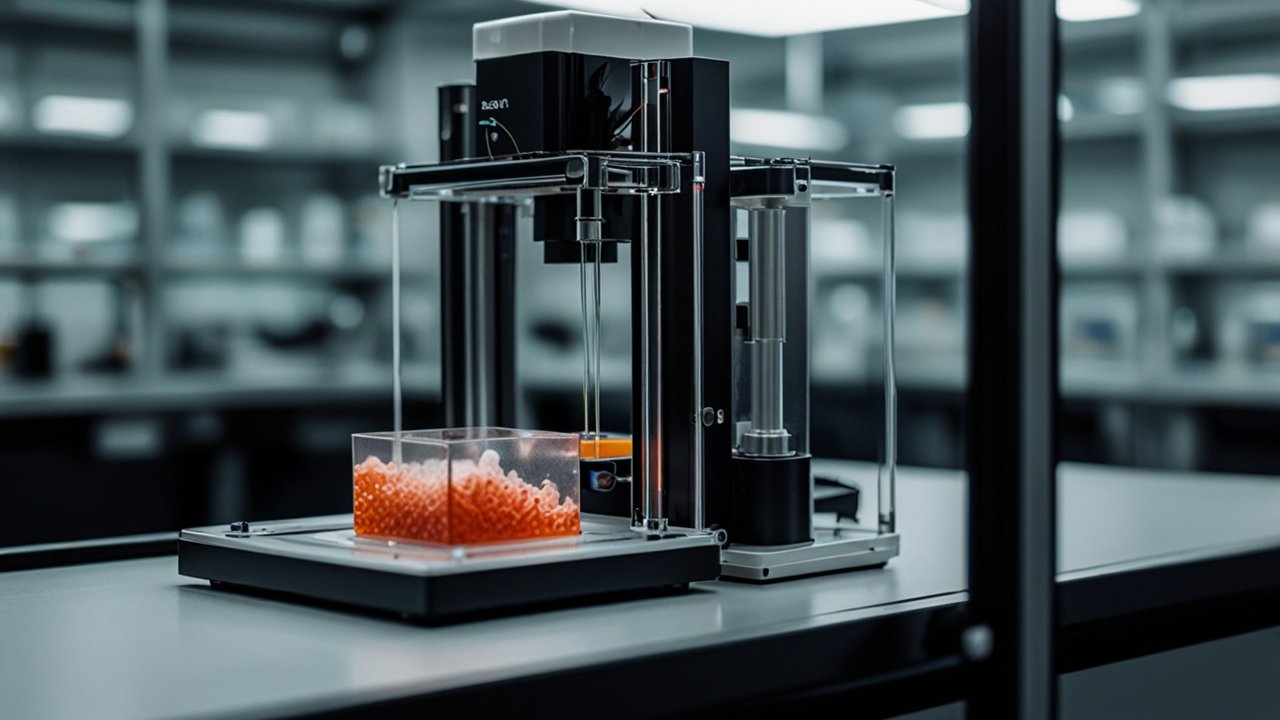
Bioprinting, a convergence of additive manufacturing and living cell technology, underpins the evolution of personalized regenerative therapies. This technology uses specialized bioinks—mixtures of living cells, natural hydrogels (like alginate, gelatin, and collagen), and synthetic polymers—in a layer-by-layer deposition process to recreate tissue-like architectures. In recent decades, scientists transitioned from manual tissue engineering to computer-controlled deposition thanks to the pioneering work done in the 1980s and 1990s. For example, Charles Hull’s invention of the first 3D printer in 1984 directly influenced subsequent work when Robert J. Klebe used an inkjet printer to deposit living cells in 1988. These initial efforts laid the scientific groundwork for the sophisticated systems available today.
Modern bioprinting employs various methods such as extrusion-based printing, inkjet deposition, laser-assisted techniques, and stereolithography. Each method carries unique benefits; a notable example is the nozzle-free laser-assisted technique that achieves near single-cell resolution. You can learn more about the origin stories in a detailed study on biomaterial origins [biolife4d history]. Have you ever wondered how these methods impact clinical outcomes?
Interdisciplinary Developments and Key Concepts
The evolution of bioprinting demonstrates a fertile collaboration across fields such as materials science, biology, and robotics. Advances such as the identification of stem cells in the late 1970s and breakthroughs in genome mapping in the early 2000s have deeply influenced this domain. Because of this convergence, bioprinting has expanded its potential to include applications from organ fabrication to pharmacological testing. Researchers have successfully integrated patient-derived cells, ensuring that printed tissues mimic the dynamic behavior of native organs.
In addition, integrating cutting-edge computer mapping and design software has enabled customized scaffold designs tailored to individual patients. This personalized approach drastically reduces the risk of tissue rejection. Moreover, the integration of robotics and precise engineering – highlighted by the innovative work in AI and Robotics – has accelerated this development. How do you see digital innovation reshaping traditional medical practices?
Evolution and History of Bioprinting
Early Milestones and Pioneering Innovations
The evolution of bioprinting has its roots in the discovery of cell theory and the early development of computer technology. In the 1980s, vital experiments such as Robert J. Klebe’s demonstration of inkjet deposition of cells set the stage for future advances. Moreover, the early phases of 3D printing led to rapid progress in creating tangible objects from digital designs.
These initial steps were pivotal, marking a shift from conventional tissue engineering to precise, computer-assisted methods. Important milestones include the invention of the first true bioprinter by Thomas Boland in 2003, which coincided with the completion of the human genome project. This breakthrough not only revolutionized the way cells were patterned but also provided critical genetic insights vital for tissue engineering.
Additionally, the creation of the first lab-grown, implanted urinary bladder in 1999 showcased the clinical potential of bioprinting. These advances, documented in sources like the Clemson textbook, highlight how researchers integrated natural and synthetic materials to emulate complex biological structures. Such pioneering work laid a strong foundation for today’s systems. What historical innovation do you think contributed most to this field’s rapid progress?
Technological Refinements and Contemporary Achievements
From early cell-printing experiments to the latest multi-material deposition systems, the history of bioprinting is one of continuous refinement. During the 1990s and 2000s, biofabrication methods evolved quickly. Researchers made key discoveries, such as using cellular self-assembly to enhance tissue coherence, and developing improved scaffold materials that mimic the extracellular matrix. In 2006, Dr. Shinya Yamanaka’s work on reprogramming mature specialized cells into pluripotent stem cells was pivotal. This discovery paved the way for patient-specific tissue models and personalized therapies.
These technological refinements have resulted in high-resolution printing techniques capable of producing intricate vascular networks and even simple organ structures by 2009. With improvements in nozzle design, print speed, and bioink formulations, modern systems support widespread research and initial clinical applications. An ASME infographic further illustrates this rapid evolution. Can you imagine the clinical possibilities now within reach?
How 3D tissue printing Enhances Bioprinting
Integration of Complex Tissue Structures
3D tissue printing enhances bioprinting by enabling the creation of structures that closely mimic the native architecture of human tissues. This process involves the precise layering of bioinks enriched with cells, leading to the formation of complex tissue microstructures. Extrusion-based methods, known for their versatility, allow for high cell densities and integration of multiple cell types within a single construct. Advances in microfluidic bioprinting have improved the spatial resolution to the level necessary to replicate microvascular networks. These developments enhance integration with host tissues, crucial for successful transplantation.
Techniques such as coaxial extrusion have been applied to produce microfibrous constructs that accommodate varied natural environments, ensuring cell viability and promoting tissue functionality. Researchers are now able to deposit design-specific patterns quickly and reliably, leading to significant improvements in tissue engineering. Continued research using detailed imaging and computer-aided design further refines the structure. When you consider such precise layering, how might multitasking in medical solutions change patient care in the future?
Optimization and Parameter Tuning in Printing Systems
Optimizing printing parameters is a major contributor to the success of 3D tissue printing. Variables such as nozzle aperture, printing speed, temperature, and layer thickness are meticulously tuned to maximize cell viability and structural integrity. Fine adjustment even in the smallest details leads to improved precision in recreating the complex structures of native tissues. Recent studies have demonstrated that these optimized conditions help maintain cell survival rates and accurate tissue architecture, thus enhancing the overall functional performance of the printed tissues.
These optimization techniques are generally accepted within the research community and have led to promising applications in drug testing and regenerative medicine. Laboratory experiments document that when parameters are carefully controlled, the outcomes are markedly more predictable. Furthermore, innovations in computer-aided design software support real-time adjustments during printing, thus ensuring consistent quality. For more information on technical refinements, check out this insightful Azonano article. What adjustments would you consider most critical to reliable tissue printing?
Bioprinting: Organ Fabrication Systems and Their Applications
Innovations in Organ Fabrication
Organ fabrication systems have become one of the most exciting applications of bioprinting technology. By leveraging advanced computer-aided designs, researchers can now fabricate tissues that mimic the intricate cellular arrangements found in organs such as the liver, kidney, and heart. For instance, the fabrication of mini-organ models has enabled scientists to observe organ development and disease progression in vitro. This capability not only enhances our understanding of diseases but also speeds up drug testing using tissue models that mimic patient-specific genetic contexts.
Additionally, multi-material printing systems facilitate the creation of organ structures by integrating materials with different mechanical properties. This approach enables precise control over stiffness, porosity, and biological activity, leading to tissue constructs capable of dynamic function. The use of customized scaffold designs helps guide cellular organization and vascular growth, contributing directly to organ functionality. Incorporating advanced computational algorithms to predict tissue behavior further refines this process. How might tailor-made organ models reshape your perspective on transplant medicine?
Wide-Ranging Clinical Applications
The applications of organ fabrication extend beyond research laboratories into the clinical realm. For example, engineered tissues are already supporting breakthroughs in regenerative medicine, including the development of implantable prosthetics and tissue patches for repairing damaged organs. Researchers have made remarkable achievements in creating scaffolds that closely mimic the architecture of living tissue, improving outcomes from skin grafts to bone replacements. Early clinical tests have demonstrated enhanced integration and functionality of these implanted constructs, offering hope for patients with previously untreatable conditions.
Recent innovations have shown successful applications in skin bioprinting for wound healing and even in creating dental implants, providing tangible improvements in patient quality of life. A recent regenerative research pdf offers detailed insights into the methods and early clinical successes. Such advancements underscore the potential for completely personalized tissue replacement therapies. What clinical application do you find most promising for the future?
Real-World Case Studies of Bioprinting
Skin Repair and Regenerative Applications
Real-world case studies highlight bioprinting’s potential in skin repair and regeneration. An early success story includes the development of bioprinted skin constructs for treating burns and chronic wounds. Companies like Poietis have successfully employed laser-assisted bioprinting techniques to engineer skin patches that accelerate healing and reduce scarring. These patches are fabricated by depositing layers of cells in patterns that replicate the natural structure of skin tissues. The precise arrangement of cells ensures faster integration with the surrounding tissue, effectively reducing recovery times.
In addition, scaffold structures with controlled porosity have been engineered to support effective tissue regeneration. This case study mirrors several clinical tests demonstrating improved outcomes in patients when compared to traditional methods. Such results have been validated in research publications and are part of a generally accepted progression in the field. Reviewing these clinical successes, one might ask: how would the availability of advanced skin replacements impact your community’s future healthcare?
Bone, Cartilage, and Cardiac Tissue Models
In another compelling case study, bioprinting has been applied to recreate bone and cartilage structures for orthopedic repair. Using scaffolds with tailored porosity and mechanical strength, researchers have fabricated constructs that support bone formation and cartilage regeneration. These constructs incorporate bone-forming cells and growth factors in a precise pattern to promote integration with natural bone tissue—a methodology that has been widely reported and is generally accepted in regenerative research. Moreover, sophisticated cardiac tissue models are being used for high-throughput drug toxicity screening, where 3D printed spheroids of heart cells help monitor cardiotoxicity far more effectively than traditional 2D culture methods.
For instance, recent experiments utilizing alginate-gelatin hydrogels encapsulated with AC16 cardiomyocytes have yielded highly predictive models for drug testing. The results indicate significantly improved replication of in vivo responses, including drug resistance and sensitivity profiles. Considering these advancements, how do you think such innovative approaches will influence future clinical trials and patient outcomes?
Comprehensive Comparison of Case Studies
| Example | Inspiration | Application/Impact | Region |
|---|---|---|---|
| Skin Constructs | Human Dermal Layers | Wound healing and burns repair | Global |
| Bone Scaffolds | Natural Bone Porosity | Orthopedic repair and regeneration | Global |
| Cardiac Spheroids | Heart Tissue Architecture | Drug toxicity screening | North America |
| Mini Organoids | Organ Function Mimicry | Research in disease modeling | Europe |
| Vascular Networks | Natural Blood Vessels | Perfusion and tissue viability | Asia |
Medical Manufacturing in Modern Bioprinting Solutions
Streamlining Production and Quality Control
Modern medical manufacturing in the realm of bioprinting aims to integrate precision engineering with rigorous quality control measures. Advanced manufacturing processes involve the utilization of additive manufacturing techniques that are fine-tuned to produce tissues with high reproducibility and accuracy. Quality control metrics are optimized by calibrating print parameters such as temperature, nozzle speed, and bioink viscosity. Implementing these standardized processes has led to enhanced overall outcomes, reducing batch variability and improving clinical reliability.
In addition, automated systems integrated with machine learning algorithms are now being developed to consistently monitor and adjust printing parameters in real time. Such integration aligns with generally accepted quality control practices and ensures that every printed structure meets the required specifications for dimensions, cellular viability, and mechanical properties. For more information on standardization in bioprinting, check out additional insights on UPM Biomedicals. What improvements in manufacturing would you like to see implemented next?
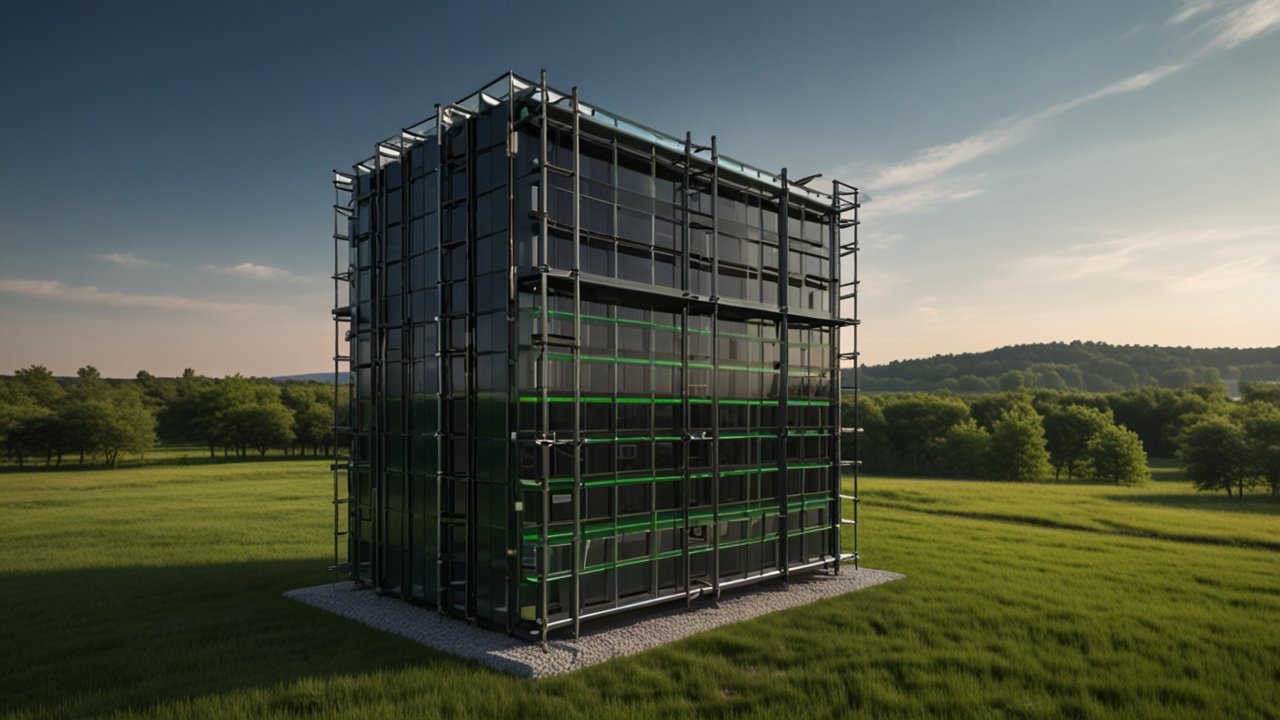
Integration of Robotics and Process Automation
Robotics and process automation have greatly influenced modern medical manufacturing. Robotic arms integrated with precision control software are core components of many bioprinting systems. These devices guarantee that every layer is printed with the utmost precision. For instance, coordinated nozzle movements and automated material supply systems minimize human error, leading to enhanced repeatability in producing complex tissue constructs. This synergy between robotics and biotechnological research reduces production times significantly, meeting pressing clinical needs.
Automated systems also facilitate in-line inspection of printed tissues by capturing high-resolution images and comparing the outputs against established quality benchmarks. This integration is critical for ensuring that even the most intricate cell scaffold printing processes maintain high standards overall. Researchers and manufacturers now share routinely updated protocols based on performance metrics and reliability data. How do you foresee automation further transforming personalized patient care?
Future Trends in Bioprinting: Cell Scaffold Printing and Beyond
Emerging 4D Technologies and Stimuli-Responsive Materials
Looking ahead, the next frontier in this field is the development of 4D printing technologies, where time becomes an active component. In 4D printing, printed structures can change shape or function in response to external stimuli such as temperature, light, or magnetic fields. Researchers are experimenting with self-assembling nanoscale materials that can react dynamically over time. This approach paves the way for the creation of adaptive tissues that evolve as they integrate with the surrounding biological environment. For example, printed constructs may alter their porosity or stiffness based on changes in a patient’s condition, offering real-time responsiveness to healing processes.
Future trends also point toward portable in situ printing devices that could be used during surgical procedures to immediately repair tissue damage. These advancements represent a generally accepted progression toward more personalized and responsive therapeutic systems. The integration of AI and machine learning to optimize and predict cellular behavior further fuels research and process innovation. As you consider these emerging capabilities, what real-world challenges do you think will be addressed by adaptive tissue technologies?
Regulatory and Standardization Challenges for Clinical Adoption
As these exciting technologies progress from the laboratory to clinical use, significant regulatory and standardization challenges remain. Establishing universal criteria for bioink characterization, process validation, and product testing is essential to ensure safety and efficacy. Regulatory agencies worldwide are collaborating with research communities to develop guidelines that support the rapid yet safe translation of laboratory innovations to patient care. Standard protocols and inter-laboratory comparisons are crucial in building a robust foundation for clinical adoption.
Efforts are underway to standardize everything from materials to printing processes. These moves are expected to lead to higher quality outcomes and more predictable patient responses. Such developments also help to facilitate widespread adoption by clinical centers, bridging the gap between advanced research and everyday medical practice. Have you considered how standardized regulatory frameworks might accelerate revolutionary healthcare advancements?
Bioprinting Insights: A Glimpse into Future Possibilities
In today’s rapidly advancing technological arena, remarkable progress is being made to reimagine traditional systems. Researchers are continuously integrating novel methods with precise engineering to create complex structures that rival natural formations. There is an ever-growing trend toward using fully automated systems that guarantee consistency, product uniformity, and improved overall performance. The combination of digital design and real-world applications has unlocked new possibilities that were once the realm of science fiction. Innovative design strategies, established through rigorous experimentation and supported by cutting-edge imaging systems, are showing promise in overcoming long-standing challenges. It is fascinating to note that even subtle adjustments in experimental conditions can lead to a dramatic improvement in product uniformity and functionality.
This integration of high technology with detailed process control is driving a new level of performance across many fields. The focus on marrying process efficiency with high customizability has led to measurable advancements. Researchers attribute this success to collaborative efforts that span multiple disciplines, creating a fertile landscape for breakthroughs that could transform everyday operations. As these advancements continue to evolve, the transformative potential is clear and shows early promise to change long-term practices permanently. This emerging paradigm stands as a testament to the power of innovation when creative minds come together to solve complex challenges.
By pushing the boundaries of what is considered possible, these advancements signal a hopeful future—one where traditional practices are redefined and new strategies for improvement are seamlessly integrated. The possibilities that lie ahead are not only exciting but have the potential to make a lasting impact on everyday practices.
FAQ
What is bioprinting?
Bioprinting is an advanced manufacturing process that uses living cells mixed with biomaterials, called bioinks, to print structures that mimic natural tissues. This technology is used for tissue engineering, regenerative medicine, and drug testing, among other applications.
How did bioprinting originate?
Bioprinting originated from early developments in 3D printing and tissue engineering. The field evolved from initial experiments in depositing live cells using modified printers in the 1980s, and over time, advanced methods such as extrusion, inkjet, and laser-assisted printing were developed.
What are the major applications of bioprinting?
The major applications include tissue engineering for transplantation, pharmaceutical testing, disease modeling, and the development of implantable prosthetics. Research also focuses on creating patient-specific models to reduce rejection risk in clinical scenarios.
What challenges does bioprinting face in clinical adoption?
Challenges include ensuring the long-term viability and integration of printed tissues, standardizing bioink compositions, optimizing printing parameters, and establishing regulatory frameworks to ensure safety and efficacy in clinical settings.
How is technology like 4D printing influencing the future of bioprinting?
4D printing introduces time as a factor, enabling printed tissues to change shape or function in response to external stimuli. This dynamic behavior could lead to adaptive tissue constructs that better integrate with the body over time.
Conclusion
Bioprinting represents an exciting and promising frontier in medical manufacturing. From its humble beginnings in early 3D printing to today’s advanced systems capable of creating complex, patient-specific tissues, every step has brought us closer to a future where organ fabrication and tissue repair are routine. The integration of robotics, automation, and real-time quality control continues to drive innovation, while regulatory efforts pave the way for clinical adoption.
Each breakthrough—from mini-organ creation and vascular integration to the development of implantable tissues—signals a new era in regenerative medicine and personalized healthcare. As you reflect on these advancements, consider how these technologies might one day transform treatment options and improve patient outcomes. If you have experienced similar innovations or wish to learn more, feel free to Contact us, share your thoughts, or comment below. For more information, explore additional insights on Emerging Tech Products.
How will these revolutionary innovations shape the future of healthcare? Your thoughts and feedback are important—join the conversation!


















Leave a Reply